Patient Access Through Self-service and Automation: Overly Complex or Just What We All Need?
More patients than ever want easy access to their own health information, including 80% of the 28 million NHS App users. This shift in priorities has contributed to the NHS’s move to enable patients to view their medical record through both its app and its other online services.
But some NHS professionals argue there’s another side to this. According to NHS Digital:
GPs will need to consider the potential impact of each entry, including documents and test results, as they add them to a patient’s record. Patients will not see personal information such as test results until they have been checked and filed, giving clinicians the chance to contact and speak to patients first.
This example epitomises the ongoing debate surrounding ‘patient democracy’ that’s reverberating around the NHS right now. Those who wish to see medical infrastructure increasingly ‘democratised’ for patients argue that better access to one’s own record helps people better understand and manage their health, leading to better health outcomes and improved satisfaction for patients and staff alike. Furthermore, as NHS Digital explains:
Automatic sharing of this information will reduce the burden on GPs long-term. They are currently required to manually share this information upon individual patient requests. The number of people who would like visibility of their records vastly outweighs the number who require limited or restricted access.
On the flipside, however, increased access to records may pose new challenges for a minority of patients, especially when it comes to safeguarding vulnerable adults, whose records may contain information that’s sensitive and confidential, which they must not themselves see, or which could put them at risk if they were unable to keep their record secure such as in cases of coercion. According to NHS Digital, ‘It may be appropriate to redact specific information entered into the GP medical record or prevent the patient from having access.’
Moreover, from the point of view of the hospital, making test results available to patients in real time without first having spoken to them could lead to panic, confusion and distress. Patients often don’t realise that their test results bring with them a greater context, which may well need explaining by a medical practitioner. This is where chatbots and virtual agents can prove immensely valuable, providing guidance and explanation about what the results mean, as well as the option to escalate to a human agent or doctor if desired.
In our view at Avaya, patient democracy should sit behind an effective triage wall, with due processes pertaining to an individual’s needs. Once the patient has passed through those rules, we believe they should then be free to control their own experience from a selection of options according to what’s most appropriate for their needs.
In other words, we advocate for a patient’s right to autonomy when it comes to their hospital experience. That means developing the digital patient experience by opening up the range of services a patient can manage themselves. This might entail automating services like appointment management, prescription management and guidance, and post-operative recovery plans and services, all using technologies such as chatbots via voice, SMS or WhatsApp. Of course, for this to happen patients would need a certain level of digital interaction with their local trust and with their own patient data. But clinicians may be wary of giving patients self-service control over various health services, especially because some patients will be predisposed to assuming the worst-case scenario without first having spoken to a medical practitioner.
This is not an easily solved conundrum, but we begin at least from our grounding premise that patients should have freedom of choice after the appropriate medical logic has been applied. There is precedent for this, too. Just look at some recent real-world high-pressure applications of this approach, like how London and West Midlands Ambulance Services have started downgrading some emergency calls to cut response times, and how some patients who call 999 are now being redirected to their GP or a treatment centre—with promising early results.
From this starting point, then, how can trusts and ICSs leverage technology to simplify their triage and escalation processes to streamline patients’ ability to find the most relevant help?
Improved patient choice and access are being delivered ‘outside the hospital’
The non-emergency service NHS 111 is an excellent example of effective decision tree use and creation, and some consider it a forerunner of an overarching movement toward greater patient autonomy or ‘democracy’. 111 takes over 1 million calls a month. That’s 1 million instances in which GPs and A&Es have been relieved of having to act as first point of contact. What’s more, 111 is now being expanded to offer increased access to specialist paediatric advice and direct access to urgent mental health support. The NHS will soon be integrating 111 into its app to further streamline patient access to non-emergency support.
The NHS will soon also be publishing more data about nearest hospitals, including wait and discharge times, to help people make informed decisions about their own care. We believe this ‘outside the hospital’ approach urgently needs emulating ‘inside the hospital’. There’s already potential for automated elements within hospital call centres, like chatbots and IVR to catch the most common ‘no treatment needed’ or ‘logistical question answered’ enquiries before an agent is dialled in. And by next winter, the NHS is looking to have increased the number of so-called ‘virtual beds’—meaning patients are monitored remotely at home—by 10,000. All of the above show the NHS’s commitment to recovering urgent and emergency care services.
Patient digital services should sit behind robust rules-based triage
Some leading voices in the NHS argue that giving patients too much control over and access to their medical records could backfire and create more chaos and confusion. This may well be true, which is why others, as well as Avaya, advocate for rules-based triage whereby the system would only ever allocate appropriate services, according to myriad ‘If this then that’ conditions, ensuring only relevant booking options are made available to the patient:
‘If patient is suffering from A and has had surgery B and medication C, they must call in to speak to an operator. If they have had medication X and operation Y, they must schedule a follow-up appointment online.’
This type of routing perfectly illustrates effective digital transformation through the connection of two or more intelligent systems which are taught to speak to one another. And by adding into the mix the electronic patient record (EHR), complete with patient self-service access, you enable intelligent systems to automate activities that previously demanded intensive administration.
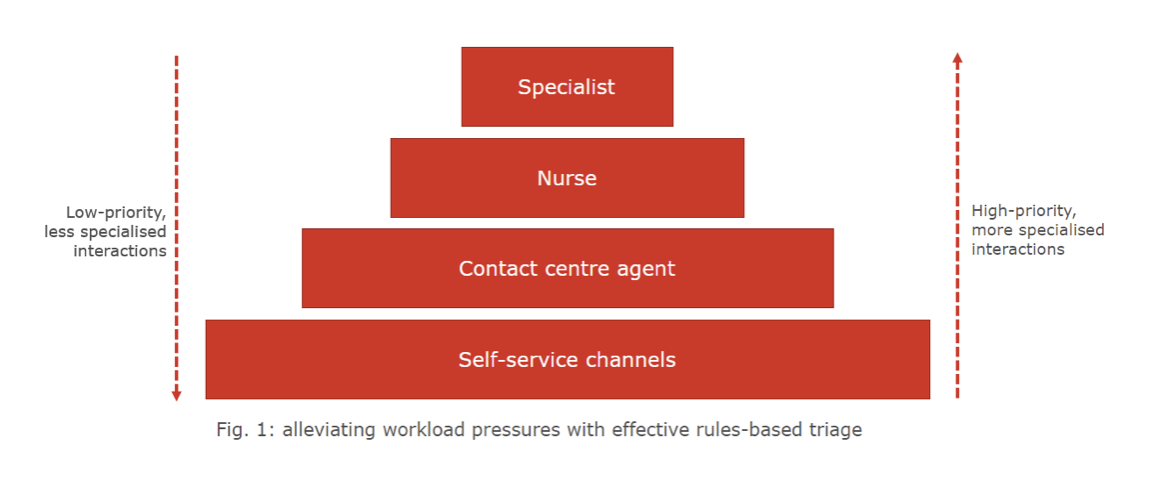
This rules-based triage makes it far easier for health organisations to shape a multichannel patient experience. As long as the rulebook can be referred to, patient self-service access can occur through any automated or semi-automated channel, like a chatbot, voice bot, IVR or WhatsApp. This increase in options is surely more attractive to the average patient than a call to a single overloaded contact centre, which could easily see them sitting on the phone for half an hour or more.
Alternatively, imagine calling a ward to check up on a loved one or enquire about visiting hours. It takes up a lot of a nurse’s time to provide families with patient updates, yet that could be all but entirely mitigated by providing digital access. Effective self-service frees up nurses, specialists and contact centre agents to deal with more complicated cases in which expert and empathetic interactions are especially critical to good patient outcomes. Staff will have more time and headspace to solve high-priority interactions effectively and efficiently, in turn improving the experience of both patient and NHS employee.
Worked example: consolidating patient access to improve patient engagement and satisfaction
A patient management services manager is concerned that the many communication channels between her hospital and its patients and primary caregivers are confusing, disjointed, and causing service delays spanning the whole organisation. Patients and relatives are contacting the hospital for different services via multiple channels, using different email addresses and different numbers for phone and SMS, with no unified coordination or data source for all patient services.
But once her organisation implements an omnichannel patient services solution to unify email addresses, phone and SMS numbers and new digital channels, patients can communicate with a one-stop shop of healthcare services within the contact centre. This prevents delays and confusion, and boosts patient satisfaction and confidence in the services they receive. And by enabling mobile service recording at the point of care, the manager’s organisation minimises patient data administration, which is now carried out by the most suitable resources as opposed to medical staff who are already rushed off their feet.
Case study: Helse Vest enables better patient care with Avaya
Helse Vest is a state-owned regional health authority operating in the second largest health region in Norway. Its patient care and access were being negatively impacted by disparate technologies:
- a lack of reporting capabilities
- a labyrinth of incongruent telecom and audio–video solutions
- ageing telecom infrastructure
- siloed technology in regional hospitals
- organisational synchronisation issues, like overlapping lunch breaks at different healthcare centres, varying reception hours at different polyclinics leading to scheduling difficulties for patients, and no automatic call handover between clinics leading to call centre coverage gaps.
“We saw different technologies increasingly merging into each other and recognised that a change in our technology was needed to reap the full benefits of a centralised IP platform.”
John Arne Lillestøl—Head of Section Telecom, Helse Vest
With Avaya, Helse Vest updated its IP infrastructure to a centralised technology platform, converted its telephony situation from traditional to IP-based technology, and introduced extensive automated reporting capabilities. The results were astounding:
- 40% reduction in call abandonment rates
- 20% increase in call processing
- shorter patient hold times
- improved staff efficiency through the elimination of redundant administrative efforts and the optimisation of skill sets
- enhanced care coordination workflows based on comprehensive near-realtime contact centre data.
The foundations laid by the upgrade to Avaya’s technology enabled vastly superior patient triage and self-service system transformed operations at Helse Vest. It would be fair to say they wonder how they ever got by before they found Avaya!
Think Connected: semi-automated patient services behind an effective rules-based system
Change is a constant in the NHS. Workflows must be adaptable to how hospitals actually operate in the day-to-day. The era of open APIs means healthcare staff, development teams and IT departments can rapidly design, test, and implement workflows as needs arise. A focus on interconnecting healthcare applications with modern communications and collaboration services ensures seamless and effortless experiences for all by accelerating the introduction of new workflows and facilitating the automation of even the most rudimentary and time-consuming administrative tasks.
With Avaya, the patient and employee experience can be designed and integrated into our communications and collaboration solution platform. Our interoperable, highly resilient and enterprise-grade architecture makes building digital workflows to transform patient care not only fast but frictionless, too, delivering experiences that ‘simply work’ for staff and patients alike. Digital-first experiences connect devices, applications, and systems, empowering trusts and ICSs to truly realise the foundational promise of digital transformation.
Determine your trust’s or ICS’s progress—and Think Connected with Avaya
Check out our vision pack to explore the array of our solutions your trust or ICS can pilot to generate far-reaching change by regaining control of its own technological path.
Download the vision pack
And to accelerate the results of your pilot, take our quick and easy healthcare Innovation Maturity Model assessment. This provides immediate recommendations and sets the benchmark for innovation readiness in terms of serving the demands of staff and patients and highlighting your position among your NHS peers. See your results against industry standards, and within days you’ll receive an overview of your organisation’s readiness and ability to achieve its goals.
Take the Innovation Maturity Model assessment
If you have any questions or would like to find out how Avaya could help your trust or ICS overcome the obstacles it faces on the way to providing first-class care and experiences for both staff and patients, don’t hesitate to contact us today!
